Blog

Diabetic Foot Infection Rate Surprisingly Reaches 98%! Master 6 Major Health Secrets to Fight Infections! The Warning Signs Behind Cracked Feet and Fungal Toenails in Diabetics
In Hong Kong, a high-pressure city with a fast-paced lifestyle, diabetes has long become a common chronic disease in urban areas. According to various medical studies, among adults over 40 years old in Hong Kong, one in every five individuals has either prediabetes or diabetes. The terrifying aspect of diabetes lies not only in unstable blood sugar levels but also in the long-term damage high blood sugar inflicts on blood vessels and nerves, leading to systemic complications. One of the most easily overlooked yet most dangerous complications is diabetic foot.
Diabetic foot refers to lower limb complications in diabetic patients caused by poor circulation and nerve damage. When the skin of diabetic feet shows dryness, cracking, or fungal nails, bacteria seize the opportunity, with an infection probability as high as 98%. If not treated promptly, it could potentially progress to cellulitis, gangrene, or even amputation. For patients, this not only results in loss of mobility but also severely impacts mental health and quality of life.

Cracked Feet and Fungal Toenails in Diabetic Patients: Don't Underestimate Small Wounds on Your Feet
Many diabetic patients initially only notice dryness, rough skin, thickening, and yellowing nails on their feet, thinking it's just a sign of aging or caused by friction from shoes. In reality, these are early warning signs of diabetic foot skin lesions. Due to nerve damage caused by diabetes, patients often have reduced sensation, making it difficult to detect minor foot wounds or infections, which can eventually develop into chronic wounds that are hard to heal.
Especially with issues like nail deformities and fungal toenails, incorrect self-trimming can lead to skin cracks, allowing bacteria to invade. Many diabetic patients thus "dare not wash their feet, dare not touch water," and even fear medical care. Over time, this increases the risk of more serious infections. Clinical observations show a rising trend in cases of cellulitis and gangrene in diabetic feet, with some patients eventually facing amputation.
The High Infection Rate of Diabetic Foot: A Close Link with Diabetes and Lower Limb Vascular Issues
The high infection rate of diabetic foot is not coincidental but rather a result of the long-term damage diabetes inflicts on blood vessels and nerves. Prolonged high blood sugar levels lead to gradual hardening and thickening of the microvascular walls, impeding blood circulation. This deprives the skin and tissues of the lower limbs of nutrients and oxygen, reducing their ability to repair. Coupled with nerve stiffness and reduced sensation, even cuts from nails or stones may go unnoticed. When this condition accompanies dry skin, fungal toenails, or skin infections, bacteria can quickly spread.Studies indicate that 15-25% of diabetic patients will experience diabetic foot wounds in their lifetime, with 20% requiring amputation due to infection or necrosis. These numbers underscore the importance of diabetic foot care, especially in Hong Kong where aging populations and the prevalence of chronic diseases increase the risk of diabetic foot complications.
Diabetic Foot Care: More Than Just Medical Attention, but "Comprehensive Lifestyle Care
Many patients believe that applying medication and bandages can resolve foot wounds, but in reality, the recovery from diabetic foot requires comprehensive management, including:
Professional wound care — Assessment of wound depth and skin condition by healthcare professionals for dressing changes, wound cleaning, and pressure relief.
Blood sugar management — Controlling blood sugar levels is fundamental in preventing worsening of wounds.
Foot pressure distribution and orthotic design — Reducing pressure on the soles to prevent new wounds.
Nutrition and foot care guidance — Teaching patients proper foot hygiene, prevention of dryness and fungal toenails, and providing nutritional advice to promote skin repair.
Psychological support and self-care rebuilding — Helping patients overcome fear of foot care, regain confidence, establish habits of active self-care.
If these care elements are managed in isolation, they often fail to achieve the desired results. Therefore, integrated professional services become the new hope for diabetic patients.
Case Study: From "Afraid to Wash Feet" to "Actively Caring for Feet"
A 60-year-old patient with diabetes for over ten years and mild residual effects from a stroke had severe skin cracking on the feet, exacerbated by ill-fitting footwear, leading to an ulcer on the sole. Upon a friend's recommendation, he visited Nu Pro Nurse Centre for a professional assessment. The nursing team promptly devised a foot wound cleaning and pressure relief care plan for him and provided personalized care guidance.Within three months, the skin around the patient's wound significantly improved, and the ulcer healing rate doubled. He not only regained confidence but also acquired correct foot care techniques and continued to receive regular home nursing services, successfully transitioning from passive care to active management.
The Golden Rules of Diabetic Foot Care
If you or a family member are facing diabetes or diabetic foot issues, remember the following guidelines:
Check your feet daily: Look for redness, swelling, blisters, cracks, or discoloration.
Use warm water to wash your feet: Avoid scalding hot water, and ensure thorough drying after washing.
Moisturize regularly: Maintain soft skin on diabetic feet to prevent cracking.
Choose shoes and socks carefully: Wear loose, breathable shoes to avoid friction.
Seek professional nursing services regularly: Have healthcare professionals inspect and guide foot care.
Manage blood sugar levels: Stable blood sugar is crucial in preventing diabetic foot complications.
By consistently following these simple lifestyle habits with the assistance of healthcare professionals, the risk of cellulitis and gangrene in diabetic feet can significantly decrease.
Nu Pro Nurse Centre: Your Health Companion
In this era of rapidly increasing healthcare needs in Hong Kong, Nu Pro Nurse Centre serves as the bridge between home care and clinical expertise. Whether it's diabetic foot care, long-term care for diabetic patients, or daily care services for the elderly, Nu Pro Nurse Centre provides personalized high-quality care solutions. They not only address patients' medical issues but also focus on enhancing overall quality of life, helping diabetic patients transition from passive treatment to active care management, truly regaining health and confidence.
Diabetic foot is not a fate but a health management challenge that can be altered. With timely detection, acceptance of professional care, and consistent monitoring, wounds can heal, and health can be restored. Diabetic patients should not fear washing their feet or touching water but should bravely understand their feet, cherish them, and care for them.
Nu Pro Nurse Centre, with professional nursing and thoughtful care services, becomes the trusted long-term health partner for diabetic patients in Hong Kong. They will continue to promote the concept of "intelligent healthcare," ensuring that every patient can feel safe at home.











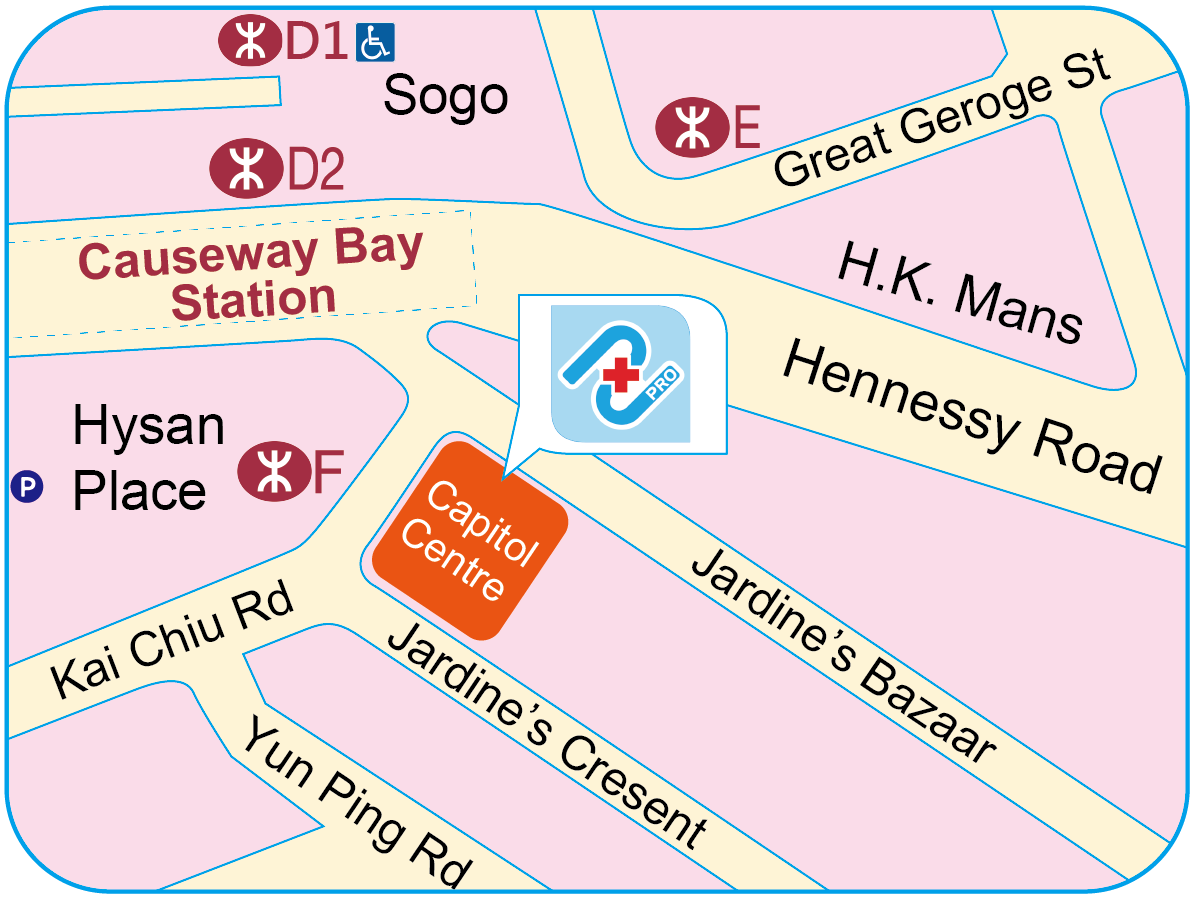
 Causeway Bay Centre
Causeway Bay Centre